Due to legal reasons set forth by the press team of our interviewee’s company, The Triangle is not allowed to release where he works. The Triangle is only allowed to release that our source, Kurt Palumbo, is an infectious diseases physician assistant working in Philadelphia.
Ethan Hermann: Thank you for being willing to discuss your experience with Philadelphia’s defense against COVID-19. It means a lot.
Kurt Palumbo: Thank you again for interviewing me. I am humbled at the opportunity. As always, the answers to your questions are reflective of my own personal opinions and do not reflect those of any one healthcare organization.
EH: As you work in Philadelphia as an infectious diseases physician assistant, what does a “normal” day look like for you? What do you find yourself doing the most for your job?
KP: A “normal” day consists of arriving to my office and following up on any outstanding patient calls, results, or messages from providers/patients from the following day. Once that is all taken care of, I primarily see patients in the outpatient clinic for either half or full days depending on the weekday.
My typical patient population are those recently discharged from the hospital, many of whom are on intravenous antibiotics with a variety of infections. For these visits, I go over their antibiotics and durations of therapy, order any necessary imaging/blood work and provide extensive counseling. In between visits, I occasionally answer patient calls, as well. Most days are fairly busy.
Now, with COVID-19, my volume of patients has decreased. I’m primarily doing telemedicine visits — either by phone or video. Any time away from patients is then spent coordinating and performing COVID-19 testing for health care workers.
EH: In a big city like Philadelphia, the spread of the novel coronavirus can happen rapidly. How do people who live in close quarters or near a lot of other people best manage themselves and protect their fellow residents?
KP: When you look at the data from China, virtually all person-to-person transmissions occurred indoors. With that in mind, social distancing is one of the best ways to help reduce the spread of COVID-19.
Limiting your exposure to other people will help reduce the chances of transmission.
This is especially important in a place like a grocery store, for example. Aisles are relatively confined and it is quite difficult to maintain six feet of separation when there are multiple people in one aisle. If you notice a lot of people in one aisle, skip it, and go get something else while you wait for the people to leave the aisle.
Masks are also beneficial in a situation like this because they help act as a physical barrier to aerosols, which is important. Aerosols take longer to dilute indoors, especially when compared to outdoors.
EH: When it comes to busting any myths that you’ve heard or read about, what are the truths that you want uninformed or misinformed people to know about the current state of this pandemic?
KP: One myth that particularly troubled me was hearing about people meeting after completing 14 days of self-quarantine, separately. The rationale behind this decision was that if both parties self-isolated, separately, then it would be safe for both groups to meet upon completion of their respective quarantines.
This is simply not true.
Unless both parties were under strict isolation and without any human contact for the 14 days, the risk — while low — is not zero percent. This then ties in to the point that a majority of patients have no infectious symptoms at all. We also do not know how long people remain infectious.
For these reasons, it is imperative that individuals remain diligent in social distancing, even after 14 days.
EH: Philadelphia being so close to New York City, of course, garners worry regarding a lot of cases and deaths. How did the medical systems in Philadelphia prepare for a large amount of cases to occur in the city?
KP: Virtually every healthcare institution in Philadelphia came up with an action plan to deal with the impending influx of patients within the health system. This involved a multi-disciplinary approach spanning both inpatient and outpatient institutions.
Some examples of this planning included establishing drive-thru testing centers, canceling elective procedures, scaling back outpatient clinics, transitioning in-person visits to telemedicine visits, utilizing operating rooms for possible ICU beds and creating designated “COVID” units within the hospital.
I speak for a majority of providers when I say we were shocked at what we saw unfold in New York City, and we wanted to do whatever we could to prevent that from happening here in Philadelphia.
EH: With Philadelphia County having almost 16,000 cases now, what is the current state of affairs regarding Philadelphia’s continuing battle against the novel coronavirus?
KP: Presently, the number of cases in Philadelphia continues to grow each day. About 1,500 new cases are reported each day to the Pennsylvania and New Jersey Departments of Health. This has been stable over the last few weeks, which is either indicative of a stable increase in the number of cases, or reflective of our maximum testing capability.
I would like to believe the former, given the percent positive rate for tests has also remained stable over the last few weeks.
EH: What is the one thing that has surprised you most about the pandemic during your time at work?
KP: This pandemic has forced many of us to get creative when it comes to taking care of our patients. It made me think critically about who really needed blood work, or a CT scan, or an MRI. Of course, sometimes you need those pieces of information to help guide your management, but I have been pleasantly surprised at the number of patients I’ve been able to take care of without these measures.
EH: If you aren’t living alone, do you find yourself a burden or a risk to your family/roommates? How do you balance that consciousness?
I think this is an interesting question. While I live alone, I still find myself to be a burden to my friends and family. The reality is that I am exposed to positive patients on an almost-daily basis.
Although I am asymptomatic currently, I could have contracted the virus during my job (or even outside of work, whether that was on a run or at the grocery store). As such, I refuse to see any of my family members in person.
I have family members who are older than 65 with underlying medical conditions that place them at a higher risk of severe illness, so I am actively avoiding them.
Although it is difficult for them (as well as myself), it is a necessary step, for now.
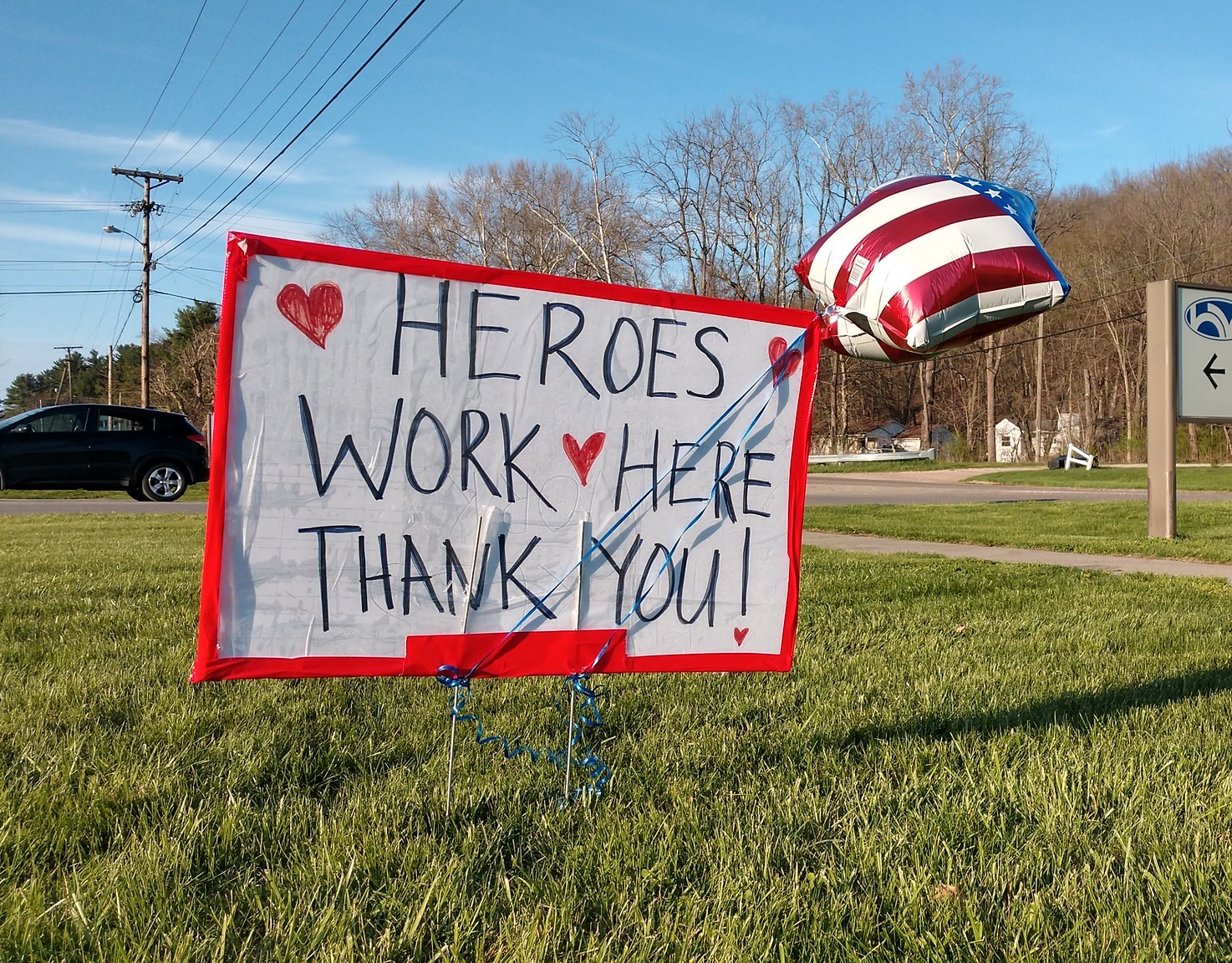
EH: Millions across the country are calling people in the medical and health professions right now “heroes.“ As someone who is working every day to fight infectious diseases, do you feel that the dubbing of “medical heroes“ glorifies the work and sacrifices being made right now by essential medical personnel?
KP: I have mixed emotions when I hear people call healthcare workers “heroes.” Although our work seems heroic, for many of us, it is simply “another day at the office.” When I graduated PA school, I swore the Hippocratic Oath, which is a medical code of ethics and asks you to treat patients to the best of your ability. For many of us, that sentiment is being tested right now.
We are taking care of sick patients to the best of our ability as we continue to learn about this disease in real-time. We work long hours and sacrifice time with our loved ones. That didn’t change before this pandemic and it won’t change after this pandemic. I don’t particularly find that to be heroic, by any measure, I just see it as a necessary part of the career I chose.
It is a privilege to participate in the health of another human being, and I feel humbled by that, now more than ever.
EH: What’s the happiest thing you’ve been able to witness since the beginning of the shutdown?
KP: As stressful as these last few months have been, I think there has been a real sense of community within our country. A majority of Americans realize their simple acts of self-isolation, mask-wearing and hand-washing have a larger impact on our community as a whole, and that has been a welcome breath of positivity.
Although these acts may feel insignificant at the individual level, they have much more power at a global level.
EH: Anything else you’d like to add, share or comment on?
KP: I would just like to remind everyone that this pandemic has affected people in vastly different ways. Cities like NYC have seen thousands of deaths, whereas some of our suburban cities have seen zero cases. Some people have lost multiple family members to this disease, whereas some people have lost no one.
For myself, these last few weeks have been some of the most stressful days of my entire career, but for some of my friends, this has been nothing more than a forced vacation at home. We all need to remember to take a step back and look at the big picture. Of course, we all want to get back to our normal lives, but we need to make sure we do that safely. It will take time, patience and empathy on all of our parts.
It takes us recognizing the fact that we might need to put our own self-interests aside, if it means stabilizing our country, and moving the pendulum back in the direction of progress.

